Vaccine Passports as a Human Right
The main way to control the pandemic, as we have all painfully found out, has been to restrict the movement of people. This stops people getting infected and infecting others. It is the justified basis for quarantine of people who have been in high risk areas, lockdown, isolation and vaccine passports.
It is the foundational ethical principle of any liberal society like Australia that the State should only restrict liberty if people represent a threat of harm to others, as John Stuart Mill famously articulated. This harm can take two forms. Firstly, it can be direct harm to other people.
Imagine you are about to board a plane (remember that…) Authorities have reason to believe you are carrying a loaded gun. They are entitled to detain you. But they are obliged to investigate whether you have a gun. And if you are not carrying a gun, they are obliged to free you and allow you to board your plane. To continue to detain you without just cause would be false imprisonment.
Having COVID is like carrying a loaded gun that can accidentally go off at any time. But if vaccines remove the bullets from the gun, they are not a risk to other people and should be free.
Vaccine passports are thus a human rights issue under conditions of lockdown like Melbourne and Sydney are experiencing (the situation is different in Europe where lockdowns have been relaxed), if vaccines reduce transmission to other people sufficiently. Vaccination removes the authority and justification to restrict people’s liberty.
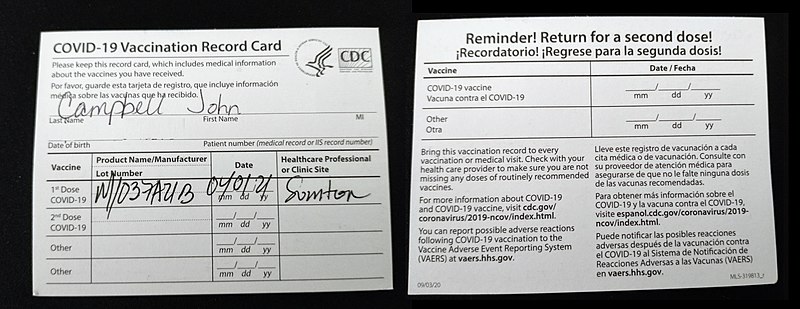
It is not discrimination to continue to restrict the liberty of the unvaccinated – it is just like quarantining those who have entered from high risk countries overseas. Their liberty is restricted because they are a threat to others. Discrimination occurs when people are treated differently on morally irrelevant grounds – differential treatment on the basis of differential threat is morally relevant. For example, to enter some countries, travellers must be vaccinated against Yellow Fever and receive a card as a vaccine passport. No card, no travel.
Are COVID Vaccine Passports a Human Right?
Do COVID vaccines fit into this justification for vaccine passports?
Read More »Ethics of Vaccine Passports