by Dominic Wilkinson, Jonathan Pugh, Julian Savulescu
Yesterday, the health secretary, Sajid Javid announced that COVID vaccines would become mandatory for frontline NHS staff from April.
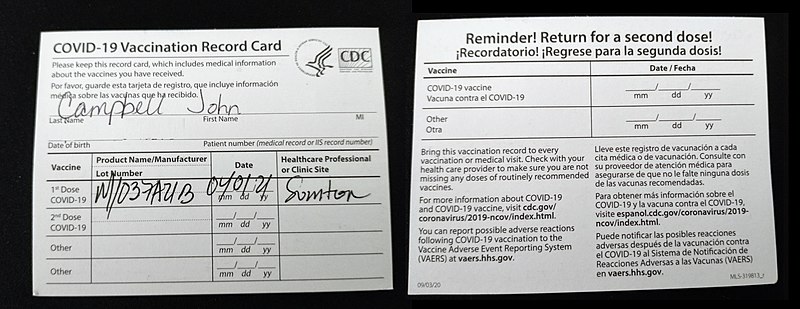
Meanwhile, from tomorrow care home workers in the UK will not be able to work if they don’t have a vaccine certificate and are not medically exempt. This vaccine mandate has been controversial, with providers raising concerns that as many 70’000 employees could leave the sector putting beds and care at risk. However, its advocates have argued that it is a proportionate public health measure due to the need to protect vulnerable care home residents.
Proportionality is one key ethical criterion in public health ethics; public health interventions are only permissible if their benefits outweigh their costs. However, another key ethical criterion is necessity; public health interventions are only permissible if they are necessary for achieving a certain benefit.
One striking feature of the current UK care home and NHS staff mandate is that it does not allow an exemption for those who have proof of natural immunity.
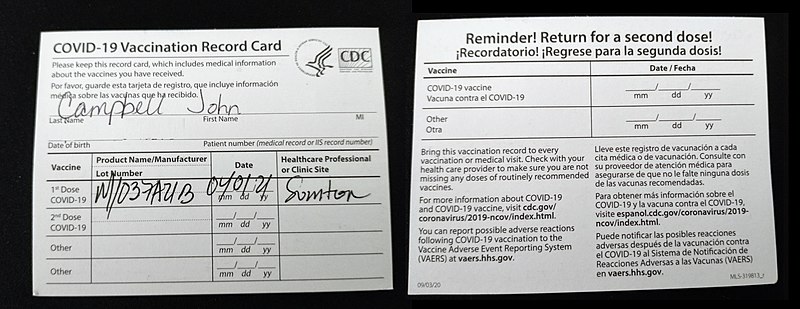
Read More »NHS and Care Home Mandates Should Take Account of Natural Immunity to COVID